
Early warning of disease exposure could improve public health responses
When a disease migrates from its point of origin to widespread geographical regions, health organizations struggle not only to treat patients but also to contain this spread. Hampering containment are the unknowns about any new disease strain — in particular, is it communicable before people exhibit symptoms and, if so, how long before the symptoms arise; how long do sufferers remain infectious; what are the best strategies for halting person-to-person infection, for treating patients?
"From an epidemiological perspective, we need a way to evaluate different disease responses," says Kajal Claypool, a senior staff researcher in Lincoln Laboratory’s Human Health and Performance Systems Group.
In a paper published on MedRxiv, an open-source, online science journal, Claypool and colleagues assess public health responses to disease outbreaks. They compared and contrasted policies typically used to contain large-scale outbreaks: self-monitoring and self-reporting, and quarantining populations, against policies that leverage technology for early detection of pathogen exposures for disease containment.
Logically, public health responses would improve with early identification of people who may have been exposed to disease-causing pathogens but have not yet shown symptoms. However, technologies that detect pre-symptomatic pathogen exposure are not yet mature enough for operational use, and the impacts of early warning on containing an outbreak and on guiding patient treatment are not well studied.
To assess several containment policies and guide further pre-symptomatic detection development, the Laboratory research team built upon a model commonly used by the epidemiological community for simulating disease outbreaks: the SEIR (susceptible, exposed, infectious, recovered) model. The SEIR model tracks a representative population through these four stages — likelihood of being susceptible to a disease, known exposure to the disease, confirmed contraction of the disease, and finally recovery. The team expanded the model by adding additional compartments for different policy choices and notional technologies deployed. The model estimates the spread of disease by solving a system of equations for various parameters, such as number of people in the scenario’s population, number of those people infected, rate of transmission, and time of quarantine.
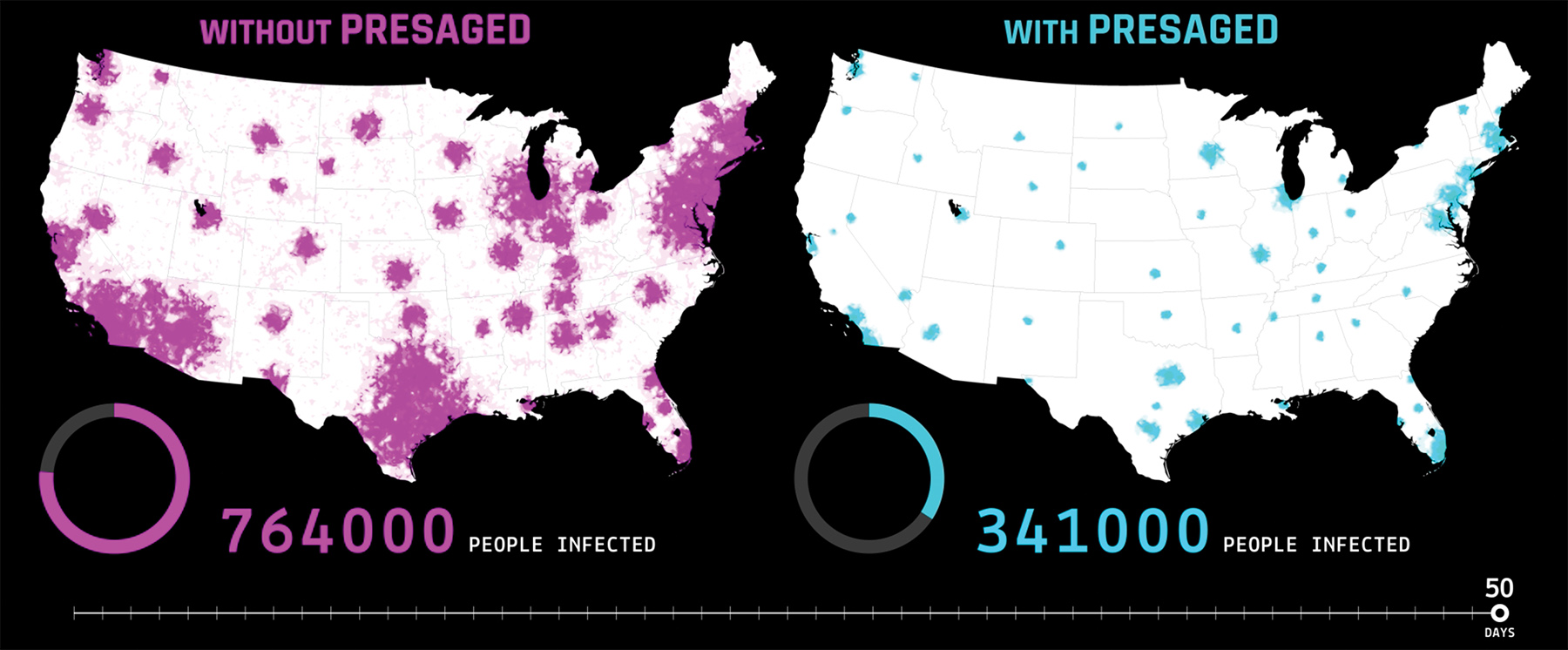
To weigh the effect of early warning of pathogen exposure on public health outcomes, the team created model response scenarios that used early warning predictions from a system called PRESAGED (for Pre-symptomatic Agent Exposure Detection) developed at Lincoln Laboratory. PRESAGED uses physiological signals to detect an individual's exposure to pathogens, such as viruses and bacteria, before overt symptoms emerge that alert patients and clinicians of potential infection. In animal (non-human primate) models, the PRESAGED algorithm was shown to provide one to three days of early warning before symptoms such as fever appear. The early warnings were not dependent on the particular pathogen, exposure route, or animal species.
"PRESAGED does not identify the specific pathogen to which a person has been exposed; it instead provides an indication that an individual is likely becoming ill so steps can be taken to inhibit the spread. Further tests could determine the specific pathogen and further inform patient care and public health policy," says Shakti Davis, a senior staff researcher in Lincoln Laboratory's Human Health and Performance Systems Group.
Findings about different public health policies
At the level of the individual patient, self-isolation and self-reporting are common responses to a disease outbreak. When the public learns of an outbreak, some people monitor themselves for symptoms, isolate themselves if they get sick, and report their illness to either their doctors or a local health agency. In calculating the impact of self-quarantine and self-reporting in the SEIR model, the team made an assumption that the isolation effectively curtails that person’s transmission of the disease. However, they determined that this response to an outbreak may have limited impact on halting its spread because by the time a symptomatic individual self-isolates, there is some likelihood that the person has already transmitted the disease.
The Laboratory researchers also evaluated the impact of quarantining everyone within an at-risk population for the duration of communicability. While this "quarantine-everyone-at-risk" response can be effective in stemming the outbreak, it comes with some undesirable costs. Healthy individuals within the quarantined group are at greater-than-normal risk of coming in contact with the pathogen as it breeds in a closed environment, leading to illness for people who may never have become ill otherwise. A quarantine-everyone-at–risk policy brings economic hardships for people who cannot go to work and lost productivity for their employers. In addition, quarantining a select group, such as everyone aboard a certain airplane flight, results in logistical expenses of housing and feeding a significant number of people.
"We evaluated the impact of a third policy that relies on technologies such as PRESAGED for detecting a person’s exposure to a pathogen before the person has overt symptoms — fever, for instance. This policy allows us to assess the economic and personal impacts of deploying early warning algorithms to gauge the probability of a person’s exposure to a virus or bacteria)." says Mark Hernandez, first author of the study.
In this quarantine-on-alert policy, people would be quarantined when an early warning system alerted that there was a high probability that an exposure had occurred. "Our calculations indicate that this is an effective, sensible response to an outbreak that mitigates the burdens of isolation and quarantine while also prioritizing possibly limited diagnostic or other medical resources," says Albert Swiston, senior author on the study and former technical staff in the Human Health and Performance Systems Group.
Quarantine-on-alert has the benefit of keeping potentially contagious individuals from spreading an infectious disease, thus reducing the spread of the disease to healthy people while minimizing quarantine costs on government, businesses, and individuals. Further, quarantine-on-alert based on objective criteria is a more reliable response than relying on individuals to recognize when to self-quarantine.
The team looked at three levels of early warning: high sensitivity (aggressive alerts with high tolerance of false positives), high specificity (conservative alerts with very low tolerance for false positives), and a near-ideal (reliable alerts with mild tolerance for false positives). The results for the quarantine-on-alert scenarios found that the elevated false positives produced in the high-sensitivity scenario meant that many individuals would be erroneously characterized as carrying a disease-causing pathogen and would be isolated unnecessarily, incurring significant unnecessary expenses. Early warnings that were highly specific for indicators do not alert enough, allowing infected people to avoid quarantine. However, an algorithm that finds a middle ground between sensitivity and specificity can generate predictions with enough accuracy to provide significant prevention of disease spread.
Need for expanded work on early warning
"We have only captured a subset of the factors that must be considered in the formulation of a rational, effective outbreak response policy," Claypool says. "The context of the scenario will ultimately inform what the ideal response for an early-warning of infection sensor would be. For example, if the consequences of infection are high, such as if the infection is almost always fatal or is associated with severe symptoms and long‐term complications, then the system might be tuned such that false negative rates are minimized at the expense of higher false positive rates," she explains further.
While the Lincoln Laboratory research has shown the value of an early warning system integrated with a larger quarantine/isolate/treatment response, more development and testing are needed before such a system becomes a standard tool in disease mitigation.
"The ability to detect pathogen exposure and possible infections well before existing methods opens incredible opportunities for blunting the impacts of an epidemic by reducing the rate of transmission and 'flattening the curve' — but much remains to be done in refining these tools for improving both public health and patient care," says Catherine Cabrera, leader of Lincoln Laboratory's Biological and Chemical Technologies Group.
As the world struggles to address the current coronavirus challenges, it seems clear that investment in technology that provides early warning of pathogen exposure would be money and time well spent — before the next threatening pandemic.